War, disasters, and infectious diseases are considered the three greatest threats to the survival of humanity. What they all have in common is the social disruption caused by the proliferation of unseen fears that accompany drastic environmental changes. In particular, environmental deterioration related to food and housing security, caused by natural disasters or infectious diseases spread by unknown viruses, is unpredictable and difficult to visualize, requiring the implementation of complex countermeasures.
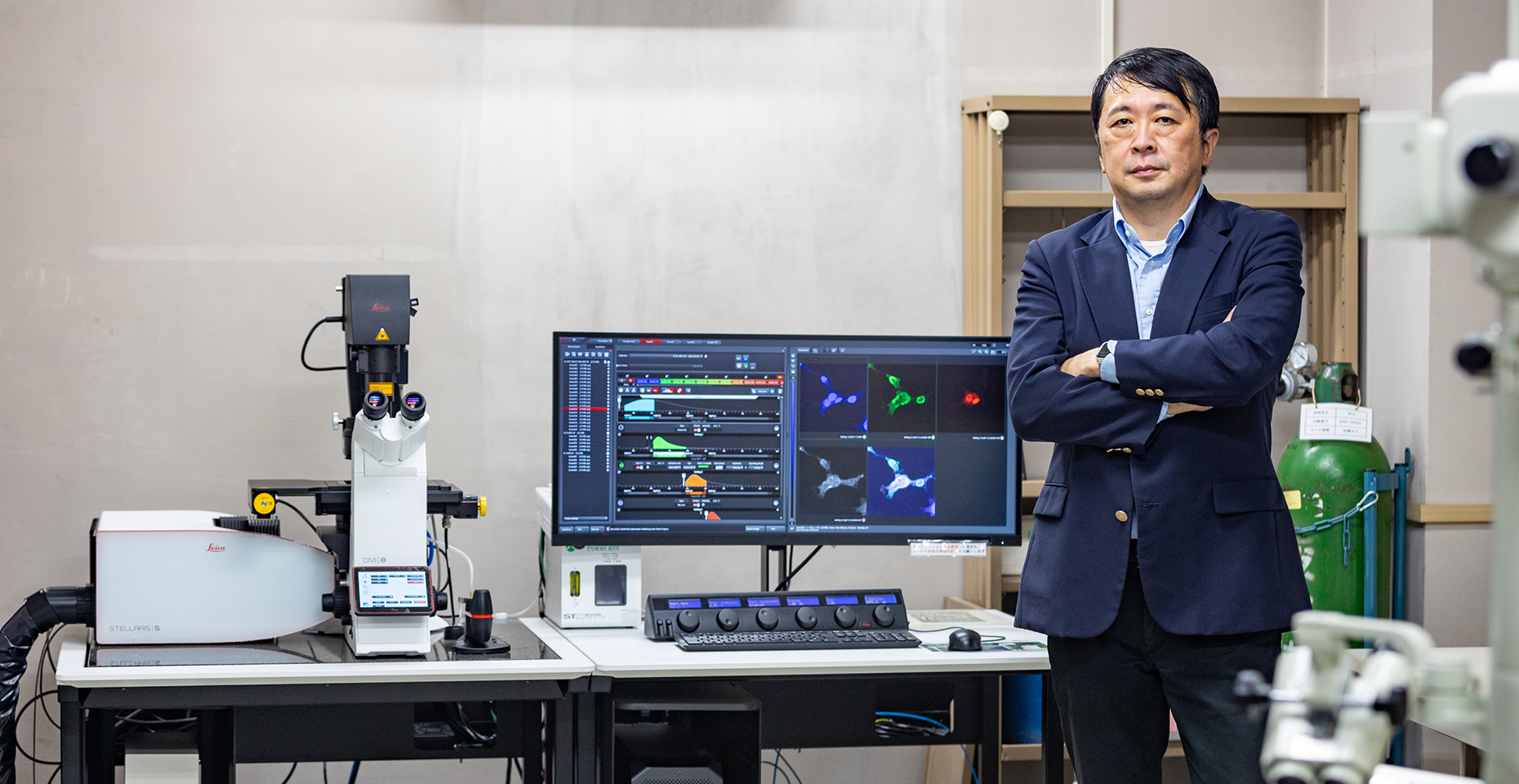
To deal with this formidable and invisible enemy, Chiba University’s Research Institute of Disaster Medicine, Division of Pandemic and Post-disaster Infectious Diseases, is boldly taking on the challenge of unraveling the mechanism behind these pathogenic challenges. We asked Professor Mitsutoshi Yoneyama, the Director of this division and Deputy Center Director of the Medical Mycology Research Center of Chiba University, about the significance of promoting research on infectious diseases at the Research Institute and the outlook for research in this area.
The reason infectious diseases are garnering attention in the midst of dealing with disasters

—To begin with, please tell us about the background of the establishment of the Division of Pandemic and Post-disaster Infectious Diseases.
One of the catalysts was Typhoon Hagibis, which caused extensive damage primarily in Chiba Prefecture in 2019. This disaster highlighted the issues concerning not only critical care during the acute response phase, such as direct injuries, but also issues that may arise in the transitional and long-term recovery phases. For example, in the realm of infectious diseases, opportunistic infectious diseases*—which attack those whose immune systems are compromised due to the overextended living conditions of a deteriorated environment in a disaster zone—became a major problem. The Research Institute of Disaster Medicine was established under the leadership of President Nakayama by bringing together researchers from various fields within Chiba University to respond to such disasters in a comprehensive manner. Division of Pandemic and Post-disaster Infectious Diseases is positioned to conduct research on infectious diseases under this context in collaboration with the Research Institute.
The pathogens that cause opportunistic infections are diverse, including viruses, bacteria, and fungi. In particular, against the backdrop of a super-aging society, infectious diseases caused by common fungi that exist around us, such as molds, are becoming an issue. Chiba University hosts the Medical Mycology Research Center, the only research facility in a national university in Japan that conducts basic and clinical research on infectious diseases caused mainly by pathogenic fungi. This is where we perform basic and clinical research on the pathogenicity and drug resistance of pathogenic fungi. We also collect and distribute isolates from patients to related researchers in Japan and overseas. Faculty members of the Medical Mycology Research Center, including myself, have begun activities in the Division of Pandemic and Post-disaster Infectious Diseases.
* Infectious diseases caused by pathogens that otherwise would not have been pathogenic under normal conditions but become pathogenic to a host with an impaired defense system.
—What was the other catalyst?
As if it were following the Typhoon Hagibis disaster, the coronavirus disease 2019 (COVID-19) arrived, and it has become—and persists as—a global-level disaster. We must prepare against situations that are created by ever-mutating viruses that pose unpredictable threats.
At the Medical Mycology Research Center, we have the only Biosafety Level 3 (BSL3)* experimental facility on campus. Initially, this facility was designed to deal with highly pathogenic class 3 fungi. While fungi are able to propagate on their own, viruses must infect cells to multiply, and thus, facilities that culture cells are indispensable. Therefore, we restructured and prepared to cope with the spread of this recent virus. As of Fall 2020, the BSL3 facility of the Medical Mycology Research Center has begun research activities dealing with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
*A laboratory capable of physically containing pathogens that cause serious illnesses in humans, such as highly pathogenic influenza, SARS, Middle East Respiratory Syndrome Coronavirus (MARS), tuberculosis, and plague.
Armed with over 70 years of tenacious fundamental research to combat “unseen enemies”

―How do we respond to disasters brought about by the unseen?
The sight of people collapsing due to the spread of something invisible to the naked eye, such as bacteria, fungi, or viruses, creates fear. There are many mechanisms that have not yet been elucidated, and with viruses that continue to mutate, like the one we are confronted with now, we do not know what the correct answer is. For this reason, the opinions of a few become strong claims, and we witness many incidences of misinformation and convictions being spread, especially on social media. In dealing with infectious diseases, in addition to the scientific mechanism approach, it is essential to take a psychological and social elements-based approach as well.
What is important is to skillfully combine daily education that encourages decision-making and actions based on data obtained from evidence-based analysis, vaccines to curb infections or the onset of disease, and therapeutics to reduce symptoms after infection.
―So, it is through this collaboration between basic and clinical research that we accumulate the insights to fight the invisible enemies, isn’t it?
We have been conducting research to fight this invisible enemy for more than 70 years. It all started around the time of food shortages, right after World War II. The Institute of Food-Microbiology was established to avoid food spoilage. Since then, we have reorganized our research divisions and hubs into the Research Institute for Chemobiodynamics, the Research Center for Pathogenic Fungi and Microbial Toxicoses, and then the Medical Mycology Research Center, which brings us to the present.
Currently, the Medical Mycology Research Center handles three types of pathogens—fungi, bacteria, and viruses*—pursuing eight projects across five fields. Also, in the two clinical divisions, we are collaborating with the Department of Infectious Diseases of the University Hospital, thereby becoming the only outpatient clinic in Japan that specializes in fungal infections and is engaged in clinical activities such as those relating to pediatric infectious diseases. Furthermore, collaboration with the Graduate Schools of Medicine or Pharmaceutical Sciences has been deepened, and basic and clinical research are being conducted in an integrated manner.
* There are three types of disease-causing pathogens: eukaryotic fungi and protozoa, prokaryotic bacteria, and viruses, which differ in their fundamental structures, methods of infection and multiplication, and size. For this reason, the countermeasures, such as vaccination and treatment methods, differ.
Collaboration with Various Fields will Further Advance Infectious Disease Research

―What kind of developments can we expect in this field in the coming future?
By the end of the fiscal year 2022, we are expecting to complete a research building at the Research Institute of Disaster Medicine with the facilities to handle the latest BSL3-level viruses. In the future, we plan to strengthen our research capabilities on infectious diseases by establishing an ABSL3 laboratory that can handle animals, such as mice.
The establishment of the institute allows for the Division of Pandemic and Post-disaster Infectious Diseases to collaborate not only with the medical field, but also with various other fields, such as information technology and sociology. It is of significance that we have established a network where researchers can connect with one another and learn about each other’s research. I am greatly looking forward to seeing what kind of research will be accelerated as we come together. Professors in the clinical field provide on-site medical treatment and take a psychological and behavioral approach to people. They are involved in educational activities such as on-site classes for junior high and high school students as well.
Personally, I am primarily conducting basic research on the responses to viral infections. In my research, in addition to developing vaccines and therapeutics for each specific virus, I am exploring highly versatile prevention and treatment methods by focusing on how immunity is regulated within the host.
―The idea of focusing on the resistance humans have seems similar to Business Contingency Plans in organizations where they take measures to ensure business continuity regardless of what kind of emergencies may arise.
We are now living in a society where the future is unpredictable due to unexpected disasters and unknown viruses. I think acquiring the mindset and knowledge to act flexibly to protect the lives and health of people—even when the cause cannot be determined—is particularly vital in such a life.
I ask myself if we can flexibly respond to and keep the proliferation of an invading virus at bay—no matter what kind they may be—by elucidating the activation mechanism of our natural antiviral activity. While this may sound like nothing but a dream, basic research is steadily and painstakingly accumulating knowledge by taking the necessary steps to realize this goal. The mRNA vaccine that appeared in the recent pandemic, which seemingly developed in a short period of time, was, in fact, the result of a global effort by researchers accumulating insights over the past 20 years.
I am hoping that the Division of Pandemic and Post-disaster Infectious Diseases will become a hub for research in various fields, such as engineering and sociology, as well as medicine, to create a resilient society against infectious diseases in disaster-stricken areas and against disaster-level pandemics. We can utilize our strengths in both basic and clinical research on various types of infectious diseases ranging from opportunistic infections to Level 3 highly pathogenic diseases. We will continue to develop our research across the departments and fields and fight against the unseen enemies of the future. We are looking for colleagues to conduct research together.
*A plan that stipulates pre- and post-disaster responses to minimize damage and not interrupt the lifeline of the organization, and to enable recovery as soon as possible, even in the event of an emergency or disaster
Series
“Disaster Medicine” to Protect our Mind and Body from Disasters
The Research Institute of Disaster Medicine aims to build a disaster medicine and nursing system in the post-corona era. In addition to researchers of medicine, pharmacy, and nursing, those of horticulture, engineering, humanities, and sociology work together to create a new society.
-
#1
2022.10.25
Creating a Pandemic-Resilient Society to Tackle Future Invisible Enemies
-

#2
2022.12.07
Shedding Light on the Public Health Nurses Working at the Front Lines of Disaster-Stricken Areas
-

#3
2022.12.12
What causes nations and regions to perceive the COVID-19 crisis differently?〜Insights from the Humanities and Social Sciences Needed for Disaster Management Research
-

#4
2022.12.20
Let Community-Based Disaster Reconstruction take roots
-

#5
2023.02.23
The role of the Research Institute of Disaster Medicine (RIDM): The indispensable research hub for urban digital transformation
-

#6
2023.02.27
Affecting behavioral changes through a combination of mind and body: How can we calmly cope with stress in the event of a disaster?
Recommend
-

Live on the Moon, Settle on Mars: Research Center for Space Agriculture and Horticulture for Space Food Production and Supply
2023.10.20
-

From Virtue to the Stars: Rethinking Education and the Universe through Virtue Ethics
2025.04.18
-

Navigating the Society-driven Research: PPI and the Quest for Research Integrity
2025.02.27