While surgery, radiation therapy, and chemotherapy have long been the mainstream of cancer treatment, the past decade has seen a surge in the popularity of immunotherapy, which utilizes the patient’s own immune system. At Chiba University Graduate School of Medicine, researchers have been exploring treatments using a type of immune cell known as ‘natural killer T cells (NKT cells).’ We spoke with Professor Shinichiro Motohashi, who leads this groundbreaking research, to delve into his thoughts on clinical trials, patient care, and the current advancements in research and development.
Japan’s first iPS cell-based cancer treatment

In 2020, your team successfully conducted the first trial of iPS-NKT cell therapy. I understand this marked Japan’s inaugural use of iPS cells in cancer treatment.
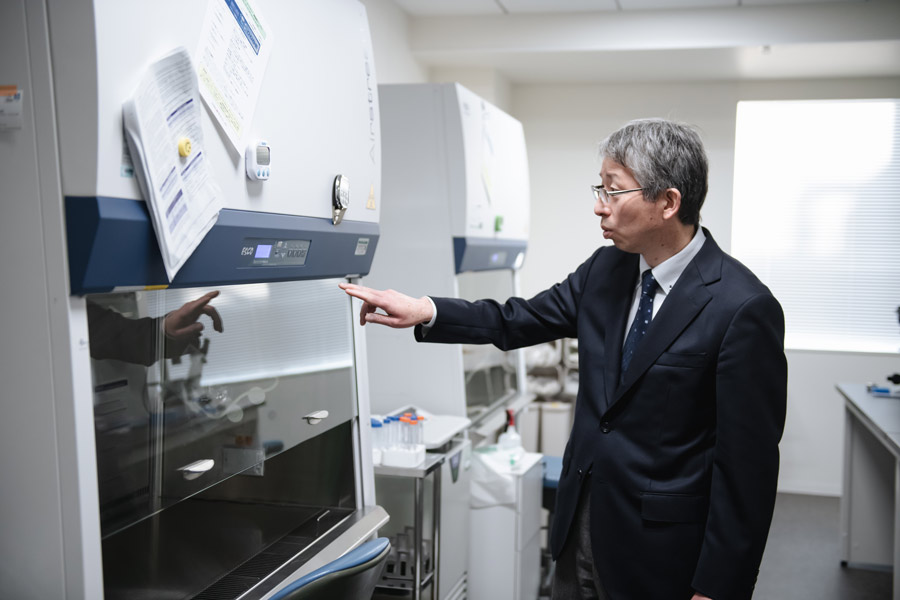
In this treatment, NKT cells obtained from the healthy individuals’ blood undergo a process called ‘reprogramming.’ During this process, the cells are transformed into ‘induced pluripotent stem cells (iPS cells),’ which possess the unique ability of pluripotency―being capable of differentiating into various types of cells through division. Subsequently, we administer these iPS-NKT cells, which are NKT cells derived from iPS cells, to patients diagnosed with head and neck cancers, including tongue and laryngeal cancers.
Why do you use NKT cells from healthy individuals and convert them into iPS cells instead of using the patient’s own cells?
This approach ensures that patients receive a consistent supply of NKT cells of sufficient quality and quantity when needed. By converting donated NKT cells from healthy individuals into iPS cells, we can produce large quantities of NKT cells with consistent quality.
NKT cells not only have the ability to directly kill cancer cells, but also to activate other immune cells. Although iPS-NKT cells are derived from donors and will eventually be cleared by the patient’s immune system, they are expected to activate numerous other immune cells, continuing the fight against cancer akin to the original cells’ mission.
This is indeed a therapy that utilizes the mechanisms of the immune system. Chiba University’s Graduate School of Medicine is renowned for its immunological research. Does it also have a long history in NKT cell therapy?
After nearly 40 years of research since the discovery of NKT cells in 1986, we have finally reached the stage of clinical trials. While groundbreaking discoveries are often made in basic research, not all of them lead to new treatments. The process of transitioning basic research findings into practical applications, including non-clinical and clinical trials, is known as ‘translational research.’ This is precisely the kind of work we do. Through translational research, many innovative treatments have progressed from basic research to practical use, although this process often takes 30 to 40 years.
During my student days, I had no intention of becoming a researcher
Have you always aspired to conduct this type of research since you were a student?
Actually, I intended to become a clinical doctor after graduation because I wanted to work in a setting where I could interact directly with patients.
However, shortly after I started working in the ward, I was called into the office of Professor Masaru Taniguchi, then dean of the Graduate School of Medicine at Chiba University and one of the discoverers of NKT cells. Showing me a photo of a mouse whose cancer had disappeared due to NKT cells, he asked me, “How about curing cancer with this?” That moment marked my entry into the world of research.
The person who nurtured me as a researcher was Professor Toshinori Nakayama, who sadly passed away recently. After obtaining my doctorate in medicine, I pursued this research under his guidance. Even after I established myself as an independent researcher, he always took the time to listen to my concerns and provide the support I needed. Without Professor Nakayama, I certainly wouldn’t be where I am today.
To encourage corporate participation in research, we conduct investigator-initiated clinical trials

I heard that your current clinical trial for iPS-NKT cell therapy is an investigator-initiated clinical trial. I have the impression that clinical trials are usually led by pharmaceutical companies.
Innovative treatments that have no precedent are difficult to predict in terms of success or failure, making it challenging for companies to readily engage with them. However, if one assesses their safety or efficacy, both research and practical application will not progress. Therefore, we physicians are conducting clinical trials first to demonstrate that these treatments are safe and effective, creating a situation where companies can consider participating.
When will this treatment be available for the general public?
Fortunately, the clinical trials have been progressing well so far. We are about to start trials to evaluate the drug’s efficacy. Even if these and other upcoming trials proceed smoothly, it will take over five years to address all the issues required for approval.
I’m sure many patients want this to happen as soon as possible.
Indeed. We are the ones who interact directly with patients on the front lines of clinical trials, facing those who desperately want new treatments as soon as possible. Every time we hear the earnest wishes of patients and their families, we feel even more strongly that we must not give up on our efforts to balance safety with the speed of drug approval.
Striving to apply this therapy to lung cancer, affecting a large number of patients


What is your future research prospect?
To further enhance the anti-cancer effect, we will soon begin clinical trials that administer another type of immune cell, ‘dendritic cells,’ along with iPS-NKT cells. Dendritic cells stimulate NKT cells, while NKT cells also activate dendritic cells, which we expect a significant synergistic effect.
In addition, using iPS cells in this treatment opens up future possibilities to introduce genes with stronger anti-cancer properties, improve cancer detection, and increase the activation of other immune cells.
Currently, we are treating only head and neck cancer, but we are developing technology to increase the number of administered cells. This will enable us to eventually treat lung cancer, which has a larger patient population.
To achieve these goals, we are advancing with the support of many, including Professor Haruhiko Koseki’s iPS cell technology, among other basic research efforts. We also benefit from support provided by the Clinical Research Center and the administrative department at Chiba University Hospital.
Translational research relies on the accumulated work of great predecessors—standing on the shoulders of a giant, allowing us, small as we are, to see distant horizons―and the presence of dedicated colleagues who tirelessly work alongside us to bring this therapy to societal application.
Making clinical trial participation a positive experience for patients

In translational research, which involves people from a variety of positions, I imagine researchers often find themselves caught between different perspectives
As a researcher, there are days when anxiety keeps me up at night, worrying about what will happen if the clinical trials do not go well. However, I also feel encouraged by the hopes of anonymous supporters who believe in iPS-NKT cell therapy and donate to support my research.
Additionally, interacting directly with patients as doctors in clinical trials allows us to feel the significance and value of our research firsthand. This kind of experience can only be gained by being on the front lines as both a researcher and a doctor.
One of the most rewarding aspects of being a doctor involved in clinical trials is learning about the needs of patients in difficult situations through our interactions with them and doing everything we can to meet those needs. Patients’ greatest wish is to be cured, but even if that doesn’t come true right away, they always have other requests. They might want to maintain a state of calm for even just one more day, or simply not want to hear that there is nothing more that can be done.
Clinical trials rely entirely on patient cooperation, so we strive to provide patients with an experience that leaves them glad they participated.
When it comes to research involving human lives, there is no room for approaches like ‘tentative’ or ‘just for now.’ If you’re going to do it, it must be with all your might―that’s my motto.